Learning Objective
- Different steps involved in processing a prescription order
The primary responsibility of a pharmacist is to safely and properly dispense medication to the patients. The manner in which a pharmacist processes a prescription order is an important aspect of his/her professional responsibilities. The important steps in processing a prescription order are described as follows:
- Receiving the prescription: It is desirable that the patient present the prescription to the pharmacist directly. This enhances the patient–pharmacist relationship. The individual receiving the prescription should be trained to accept the prescription in a professional manner. While receiving or reading the prescription, the pharmacist should not show any signs of confusion or surprise, as it may cause anxiety in the patient.
- Reading and checking the prescription: The prescription order should be read completely and carefully in the privacy of the prescription department. Any doubt regarding the prescription should be cleared by consulting a fellow pharmacist, the prescriber, or even by checking the posological table.A pharmacist should never guess the meaning of a distinct word or unrecognized abbreviation. If any important data is omitted, it should be verified by contacting the prescriber.Sometimes, the prescriptions are received by a senior pharmacist over telephone. In such cases, the prescription should be immediately written down and should be verified by repeating it. This is important because there are a number of drugs with the same pronunciation, for example, Digoxin and Digitoxin.
- Collecting and weighing the ingredients: Once the procedure for the formulation is decided, the pharmacist assembles the necessary materials in a single location on the prescription counter. As each ingredient is used, it is transferred to another location away from the workstation. The use of this technique provides the pharmacist with a mechanical check on the introduction of each ingredient.Through this process, the pharmacist has the opportunity to read the label of each ingredient three times—once when the container is removed from the shelf, again when the contents are weighed and measured, and finally when the container is returned to the shelf.
- Preparing the prescription: After reading and checking the prescription, the pharmacist should decide on the exact procedure to be followed in dispensing or compounding the ingredients.Most prescriptions call for dispensing medications already formulated into dosage forms by pharmaceutical manufacturers. Care must be exercised by the pharmacist to ensure that the product dispensed is of the prescribed dosage form, strength, and number of dosage units.The pharmacist should verify the manufacturer’s label by comparing it with the prescription order before and after filling the order to ascertain its correctness. Products that show signs of poor manufacturing, have undergone deterioration, or have crossed the expiry date as stated on the label should never be dispensed.For prescriptions that need compounding, the pharmacist must acquire and maintain the knowledge and skills necessary to accurately prepare them. The pharmacist should also take into consideration the compatibility of all the ingredients, the right order of mixing, the need for special adjuvants/additives or techniques, and the mathematical calculations to be followed.Any calculations or compounding information that would be useful in refilling the prescription at a later date should be noted on either the face or back of the prescription order. The adjuvants used in the formulation, order of mixing, quantity of each ingredient, capsule size used, type and size of the container, name and product identification number of the manufacturer, auxiliary labels used, clarification of illegible words or numbers, price charged, and any special notations should be recorded. Failure to do this may result in difference in the appearance of the prescription when refilled and possibly create doubt and apprehension in the mind of the patient.
- Packaging: In filling a prescription, the pharmacist may select a container from among various shapes, sizes, mouth openings, colors, and compositions. Selection is based primarily on the type and quantity of medication to be dispensed and the method of its use. Table 2.2 illustrates a few examples for container selection. Table 2.2 Types of Containers for Different ProductsType of ContainerType of ProductRound vialsSolid dosage forms such as tablets and capsulesPrescription bottlesLiquids of low viscosityWide-mouthed bottlesBulk powders, large quantities of tablets and capsules, and viscous liquidsDropper bottlesOphthalmic, nasal, ear, or oral liquids to be administered by dropOintment jars and collapsible tubesSemisolids such as creams and ointmentsMost of the prescription containers are usually available in colorless or amber-colored glass or plastic containers. However, amber-colored containers are most widely used because they provide maximum protection to their contents against photochemical deterioration.
- Labeling: The prescription label is usually prepared by the pharmacist. The label should be aesthetic and professional in appearance. The size of the label should be appropriate to the size of the container and should be written or typed in indelible ink.The label contains the following information:
- Name and address of the pharmacy
- Prescription number
- Prescriber name
- Patient’s name, directions for use, and the date of dispensing
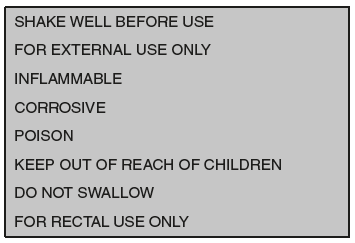 Figure 2.3 Auxiliary Labels
Figure 2.3 Auxiliary Labels - Rechecking: Every prescription should be rechecked and the ingredients and amounts verified. All details on the label should be rechecked to verify the directions given, patient’s name, prescription number, date, and prescriber’s name.
- Dispensing and patient counseling: While delivering the prescription to the patient, the instructions on the label should be reinforced to the patient.
- Recording and filing: A record of all the dispensed prescriptions should be maintained in the pharmacy by using prescription files.
Leave a Reply